Following a health scare in 2017, Andy Mellon writes this fascinating piece about the heart and what we can do to look after it.
The club training session on Thursday, December 21st was a funny one for me. I had slept badly, not eaten well that day and felt a bit flat.
As I warmed up I felt great, having to knock back the pace to avoid going too fast. I even mentioned to John Hurse that I felt a bit weird, a bit on / off during the session, but reassured him I felt well. It was probably the single best training session of the last 6 months. I relaxed at home with some food and a couple of bottles of beer over the evening before bed. The next day I was conscious of noticing a few strong heart beats, not that unusual as I’d had a few back in October which settled as I got over a minor virus infection.
I work in a hospital in Sunderland. I had mentioned the “palpitations” from October to a colleague the week before who told me that “speaking as an ex-cardiology nurse” you need to go and see your GP. As a doctor I probably shouldn’t have needed that prompt. I arranged an appointment to see my GP and got an electrical recording of my heart (ECG) done to take along on 22nd December. I was vaguely aware of intermittent fluttery feelings in my chest but I didn’t have chest pain, I wasn’t short of breath, I didn’t feel faint or dizzy or weak. I thought the ECG would probably show a few extra beats (ectopics) which are relatively common. A quick look at the recording was all it took to change everything. This was a condition called Atrial Fibrillation (AF).
CBD is the acronym for cannabidiol. It has been used by people for a long time and helps to get rid of the symptoms of many common ailments. Recently it was found that a number of common problems such as lack of cognitive abilities, mental disorders, anxiety, and both internal and external pain can be relieved by the use of CBD oil in any form. CBD is extracted from the marijuana plant but it is not psychoactive in nature due to the absence of tetrahydrocannabinol (THC). Many consumers prefer the use of CBD oil over normal medications due to its quick impact and fast recovery from the troubling symptoms. Here you can Buy full spectrum CBD oil.
You get to enjoy a sense of calmness and more focus. CBD affects learning positively and it also motivates learning. It is also helpful in reversing the symptoms of the Alzheimer disease. You can get a heart that is healthier by the use of the CBD. CBD has a lot of benefits that it brings to the heart, these include the capability of lowering high levels of blood pressure. You also get relief from the stresses that are part of your daily life. CBD has been known to provide therapeutic cures for symptoms like stress and anxiety, thus helping in the reduction of psychological levels of anxious behavior. It also helps in reducing the feeling of depression and anxiety.
Before I had time to really think about it I was reviewed by the cardiology team and given a new plan, not what I had expected for week 2 of my Manchester Marathon training programme. The rhythm has gone back to normal at the cost of going onto two drugs – one to slow the heart, the other to prevent abnormal blood clotting which can occur within the heart in this condition and which is the main source of serious complications in AF, which includes stroke – blood clot blocking blood vessels in the brain. My risk for that is low based on a commonly used calculation called CHAD score, but as they weren’t absolutely sure how long I had been in AF, treatment was recommended as “sometimes when the heart reverts to a normal rhythm that’s when blood clots get dislodged from within the atrium”.
So the end of week 1 of marathon training for Manchester became the end of marathon training full stop and I am in the process of re-evaluating my longer term goals. The more I read about the effect of exercise on the heart the more I’m having to balance what I want from my running with what I want from the rest of my life. For reasons that will become clear I have stopped drinking any alcohol, am ensuring I get to bed at a time that will allow me 7-9 hours sleep and trying to avoid eating late in the evening. I know that there have been others close in age to me (57) at the club who have had heart problems over the last year, and that some of their experiences have been far more frightening than mine. We all share a few things in common though – we are older athletes who feel pretty healthy and are pushing ourselves way beyond what is usual in people our age. That can almost feel like a badge of honour and not something I want to knock. I guess though we will all have asked the following questions: Why me? Why now? When will I or will I be able to get back to doing what I was doing before? I thought it might be useful to others to share something of my experience but more importantly to share some of the things I have learnt.
If you are interested there is a very helpful article that talks about heart rhythm in endurance athletes at the following link: http://www.velonews.com/cycling-to-extremes-heart-health-and-endurance-sports
The same authors have written a book published just last year (2017) on the subject of heart rhythm problems and older endurance athletes – The Haywire Heart (How too much exercise can kill you, and what you can do to protect your heart) Dr. John Mandrola and Lennard Zinn and Chris Case. The sub title is dramatic, as one medical reviewer has pointed out, but the book intends to help athletes understand the rather complicated research that has been carried out in this field and make choices about their own activity and what they should do to protect their heart.
I tell families all the time that knowledge is power, but sometimes that knowledge can be the last thing you want to hear. “I am going to give you choices of treatment, none of which would be things you would want to have to choose.” I feel a bit like that in writing this piece for a group of athletes who feel “young at heart”. Anyway read on if you want some more information about both normal and abnormal heart rhythms, but if you choose not to read on PLEASE listen to your body and don’t ignore potentially important early warning signals.
As endurance athletes who are ageing (that means all of us) moderate exercise levels significantly DECREASE our risk of the major type of heart disease (coronary artery disease) BUT if we are doing more intense levels of exercise we have a 5 fold increased risk of the problem (AF) I have developed compared to non-endurance athletes or the population generally.
Listen to your heart
There are other heart problems that exercise may uncover or contribute to. The following are questions recommended as part of a screening questionnaire from the American Heart Association for athletes to ask themselves about their cardiac health. The questions are less discriminating as a screening tool than more intense assessment – including ECG, Exercise stress testing, prolonged rhythm testing and ultrasound of the heart, but if you answer YES to any of them you should seriously consider discussing this with your GP with the potential for ECG, simple blood tests and perhaps involvement of a cardiologist.
Family History
- Premature sudden cardiac death
- Heart disease in surviving relatives less than 50 years old
Personal History
- Heart murmur
- Systemic hypertension (raised blood pressure)
- Fatigue
- Syncope/near-syncope (faint/ unexpected light headedness/ unexplained passing out)
- Excessive/unexplained exertional dyspnea (shortness of breath beyond expected or not settling on rest)
- Exertional chest pain (classically central, crushing chest pain, pain into left arm or jaw, but can vary in nature)
Physical Examination – This would be useful to discuss with your GP who may well not be aware of this guidance
- Heart murmur (supine/standing*)
- Femoral arterial pulses (to exclude coarctation of aorta)
- Stigmata of Marfan syndrome –
- Brachial blood pressure measurement (sitting)
How does the heart work?
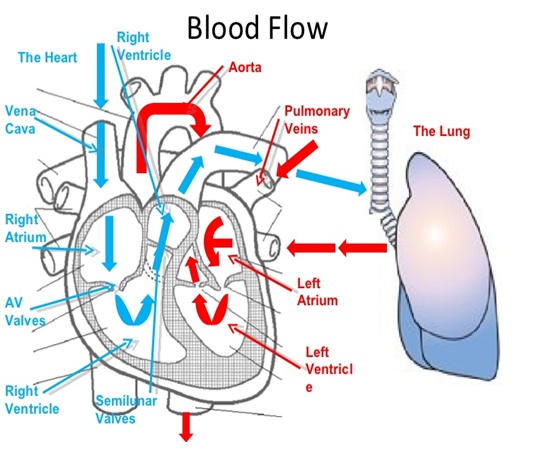 The heart has four chambers, two on the right and two on the left. Each side has a priming pump, the atrium, and a main pumping chamber, the ventricle. These are set up to beat in a constant order: atrium then ventricle, and keep doing that for a lifetime. Fibrillation refers to an altered form of muscle activity – quivering rather than contracting. If your ventricles go in to fibrillation (VF) you have no output from the heart and without CPR & electrical defibrillation to kick start them you will die very quickly. If your atria start to fibrillate you may notice your heart rate speed up, you may feel short of breath or dizzy, you may find yourself unable to keep on running, you may feel an odd fluttering in your chest or you may be unaware of anything. But you will carry on filling the ventricles and they will keep on pumping blood around your body.
The heart has four chambers, two on the right and two on the left. Each side has a priming pump, the atrium, and a main pumping chamber, the ventricle. These are set up to beat in a constant order: atrium then ventricle, and keep doing that for a lifetime. Fibrillation refers to an altered form of muscle activity – quivering rather than contracting. If your ventricles go in to fibrillation (VF) you have no output from the heart and without CPR & electrical defibrillation to kick start them you will die very quickly. If your atria start to fibrillate you may notice your heart rate speed up, you may feel short of breath or dizzy, you may find yourself unable to keep on running, you may feel an odd fluttering in your chest or you may be unaware of anything. But you will carry on filling the ventricles and they will keep on pumping blood around your body.
For an ultrasound view of the chambers pumping go to https://www.youtube.com/watch?v=7TWu0_Gklzo
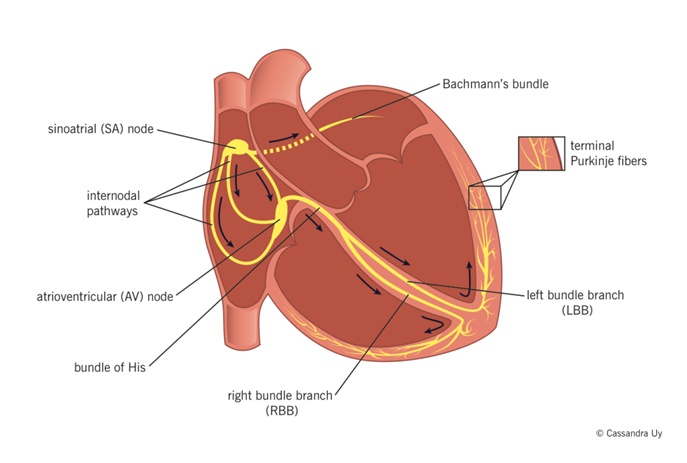
How does the electrical signalling in the heart work?
The natural pacemaker that provides regular signals to the rest of the heart is found in the right atrium (SA node) and it transmits these electrical signals first to the rest of the right and the left atrium, before the signals progress down the muscular wall between the 2 ventricles to cause near simultaneous contraction of both ventricles. The right ventricle sends blood to the lung to be oxygenated, the left receives and then sends oxygen rich blood from the lungs to the rest of the body – muscles, heart, brain, etc.
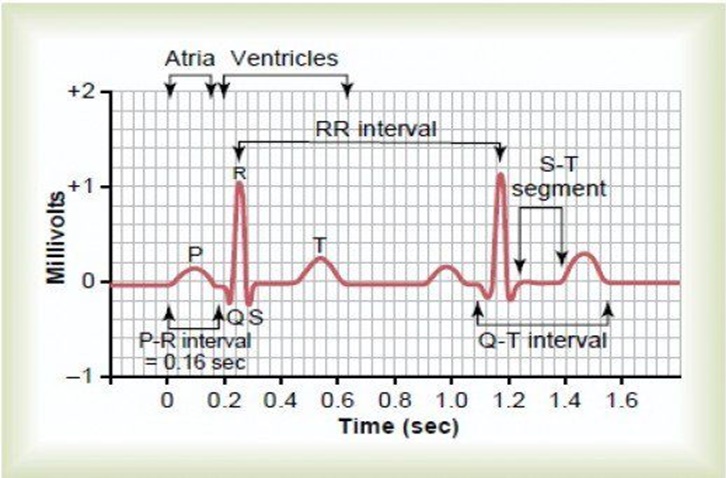
What does a normal pattern of electrical activity look like?
A normal recording of electrical activity in the heart looks like this. The electrical signal of atrial contraction is the P wave. The signal of ventricular activity is the QRS wave, and there is a recovery phase between heart beats, the T wave. If you ever have an ECG performed these are the squiggles you will see. The normal ECG shows a variation of these three wave forms across the various chest and limb leads that are used to record it.
What does Atrial fibrillation look like on ECG?
Atrial fibrillation (AF) occurs when there is erratic and uncoordinated electrical activity, rather than neat P waves being generated within the muscular wall of the atrium. The heart is usually very good at coordinating the transmission of beats to the ventricles so that the 1:1 coordinated contraction of atria (P) and ventricles (QRS) is maintained (bottom line of diagram).
This normal pattern is called sinus rhythm. The top line shows what happens when chaotic activity is happening in the atria. Signals are transmitted in a much more haphazard way than usual and this results in a faster heart rate than normal, but with a noticeably irregular pulse rate. Each of the larger QRS waves will be associated with a pulsation that can be recognised when feeling an artery.
Because the atria are not contracting, filling of the ventricles is up to 20% less efficient. Longer or shorter periods of filling of the ventricles will lead to stronger or weaker output from the heart, which in turn leads to feelings of fluttering or palpitation in the chest.
https://www.youtube.com/watch?v=9FUpBVF8xOE
Is an athlete with AF unhealthy?
Atrial fibrillation is a common heart arrhythmia usually associated with advanced age, high blood pressure, diabetes, obesity or structural changes in the heart. Exercise training in general has been associated with a reduced risk of atrial fibrillation and associated complications. However, more strenuous endurance exercise (e.g., marathon running) appears to increase the risk of paroxysmal atrial fibrillation (i.e. sudden onset periods of abnormal electrical activity) in otherwise healthy young or middle-aged athletes with no cardiac structural abnormality. Rates of AF in endurance athletes are 2–10 times greater than expected in the general population. The greater the duration and lifetime hours of activity, the higher this risk becomes.
This is not intended to be a depressing read but a realistic one that I hope may keep you well and help you monitor this important aspect of your own health while participating in the sport you have chosen.
Diabetes is a group of diseases characterized by high blood sugar levels that result from defects in the body’s ability to produce or use insulin. It is important to take and keep control of blood sugar levels in the body because when too much sugar stays in the blood, it will damage the blood vessels and nerves. Much of the food that is eaten daily is turned into sugar in the blood to be use by the body for energy. Insulin is a hormone produced in the body by the pancreas that helps the sugar in the blood get into the cells of the body. When the body doesn’t make enough insulin, or if the insulin it does make does not work properly, blood sugar cannot get into the body’s cells and instead stays in the blood, raising the blood sugar level.
Records have been documenting the diabetes disease for thousands of years. The first known recorded mention of the disease was as early as 1552 BC by a physician in Egypt. Physicians did not begin to gain a better understanding of diabetes until 150 AD when further studies were accomplished by a Greek physician. The use of insulin to treat a human with diabetes occurred in 1920 when it was determined that diabetes was related to high blood sugar levels and that insulin was a lowering agent. Today it is estimated that there are over 150 million people suffering from diabetes and in the United States it accounts for approximately 1/3 of all medical costs.
High sugar levels and damaged blood vessels cause a vast amount of complications that come with diabetes. Some of these complications can be kidney disease or kidney failure, stroke, heart attack, loss of vision or blindness, immune system suppression, nerve damage and poor blood circulation. The diagnosis of diabetes is based in an arbitrary cut-off point for the body’s blood sugar level that should be 70 – 130 (mg/dL) before meals and less than 180 mg/dL two hours after meals. Blood sugar levels for diabetics are confusing because while there are set standards, most every health care professional visited may provide different numbers to go by. The best thing to do is to take the first set of numbers received and stick to them.
The main types of diabetes are Type 1 and Type 2 with the most common form being Type 2. Approximately 90 to 95 percent of people with diabetes are diagnosed as Type 2 diabetics. In people with Type 1 diabetes, the pancreas no longer produces insulin and most often occurs at an early age. Most Type 2 diabetics can control their disease with a healthy diet, exercise, medications and supplements. One of the many medications that can be effective in controlling diabetes is insulin.
The Sunergetic Products Blood Sugar Support supplements can also be a help for diabetics. These supplements contain a combination of vitamins, minerals and herbs that are designed to help keep blood sugar levels at a safe level.
To allow blood sugar (glucose) to get into the body’s cells, insulin must be present. Insulin is a hormone produced by the pancreas, a large gland located behind the stomach. Insulin is secreted by groups of cells within the pancreas called islet cells. It is necessary for the body to change glucose into energy. When glucose stays in the bloodstream it cannot be used as energy and causes many problems. Insulin causes cells in the liver, muscle and tissues to receive glucose from the blood where it is stored as glycogen in the liver and muscle. This stored insulin stops the use of fat as a source of energy. Insulin has been shown to enhance learning and memory, and it benefits verbal memory.
The pancreas normally produces the correct amount of insulin automatically and moves glucose from the bloodstream into the body’s cells where it has extensive effects on metabolism and other body functions. Insulin injections are required when the pancreas produces insulin that is not effective, produces too little insulin or does not produce insulin. Most blood sugar problems, such as headaches, fatigue, mood swings and depression, obesity, alcoholism and diabetes can be directly related to the pancreas. Most cells in the body have insulin receptors which bind the insulin that is in the blood circulation. Cells have insulin attached to their surface that activates other receptors designed to absorb glucose from the bloodstream into the inside of the cell.
Most medical professionals will start their Type 2 patents on pills before prescribing insulin. The starting of insulin depends on several factors that include the length of time being a diabetic, blood sugar level, current medications and the patents overall health. It has been found that pills help the body make better use of insulin.
The ingredients in each capsule have been carefully chosen for its unique properties and positive and proven effects. Along with weight watching, a low fat/ high fiber diet and exercising, these natural blood sugar capsules can help in controlling blood sugar.
Why are endurance athletes more prone to AF?
- Vagal Atrial Fibrillation
The vagus nerve is the main nerve responsible for slowing the heart rate. Known vagus nerve stimulants include eating, sleeping, relaxation following stress and exercise, acid reflux and alcohol consumption.Athletes have some evidence of greater activity of the vagus nerve, which probably contributes to the slower heart rates and lesse nerve pain as seen in trained athletes. As per the review on www.thememorialhospital.org/nerve-renew-review/ anyone suffering from nerve damage or pain can most certainly opt for the use of Nerve Renew, as it is an excellent supplement which rapidly numbs pain and promotes the fixing of the damaged nerves. Many of the vagus nerve stimulants listed are common among athletes. Surprisingly there doesn’t seem to be strong evidence for caffeine affecting the risk of AF occurring although it is an area where most papers advise some caution. Alcohol seems to be an independent risk factor which increases as alcohol consumption increases. My reading of the evidence is that ANY alcohol increases the risk of AF occurring or recurring, which is why I have stopped completely.
- Inflammation
There is some evidence that increased levels of inflammation in the body can be associated with atrial inflammation and subsequently greater degrees of fibrosis (healing response with scar tissue) affecting the heart muscle and electrical conducting pathways. There is evidence of this occurring more commonly in endurance athletes.
- Enlargement of the left atrium and alternative pacemakers
As part of the response to exercise there is some natural thickening of heart muscle. This may be associated with slight distension of the left atrium. These effects can change the natural route electrical signals take through the heart and allow new rhythms to emerge that become alternative pacemakers and compete with the main pacemaker in the right atrium.
What does your own pulse feel like?
Feel your own pulse either at your wrist or the side of your neck just below the angle of your jaw (gently). As “honed” athletes it should be nice and steady and probably slower than most of your friends’. If you take deep breaths that may lead to some speeding up and slowing down of your heart rate which is normal, but at rest with gentle breathing it should be very regular. My experience was that my heart was “galloping” along at 77 beats per minute compared to a usual rate of about 45. My cardiologist thinks fitness was masking some of the effects many patients feel. Heart rates over 100 at rest are not unusual in AF. If your pulse feels irregular you should go and get it checked out – can you get to see your GP today? If not, or if you can feel persistent fluttering in your chest or are getting odd thumps in the chest, you should go to a walk in centre or A&E and get it seen to straight away so you can get an ECG done during a time of symptoms.
What can palpitations feel like?
It is not unusual to have an occasional stronger beat quite naturally – so called ectopic beats. These are commonly felt as a painless thump or bump in the chest and usually occur when the ventricle is delayed in receiving its electrical signal and has longer to fill and then pumps blood out more forcibly than usual. They are commoner when people are tired or after strong coffee. It is really important to recognise that if the pulse is irregular or feels very fast or it is associated with chest pain, feeling faint or short of breath, or ectopic beats are happening in runs of 4-5 in a row you should get it checked out urgently. If AF develops during exercise you may suddenly feel a change in your ability to push your effort, or more short of breath than expected, and this may not settle as usual on stopping exercise.
What are the outcomes if you do ever develop AF?
The best outcome is that the rhythm disturbance goes back to normal spontaneously. If it was clear that the rhythm had only just changed I would have been advised to have a cardioversion. This is the same as happens in resuscitation with VF by stimulating the heart with an externally applied electric shock, but is done under a short anaesthetic. The aim is to get the heart into a normal rhythm before it starts to become fixed in AF. The hope is that an episode does not recur but the reality is if it’s happened once you are at greater risk of AF becoming recurrent or persistent. Slowing down the heart rate with drugs (beta blockers) can be helpful but will limit exercise ability as they reduce your ability to push up heart rate during exercise. Depending on the level of risk of blood clots forming (CHAD score) you may be advised to use an anticoagulant (blood thinner) which increasingly is a newer type that doesn’t need repeated blood test checking. Sometimes other drugs are used, but if the problem becomes recurrent or persistent in younger people cardiologists will consider doing a procedure called an ablation. This means mapping the heart’s electrical activity more closely both externally and also internally through a method that involves passing a probe through a blood vessel into the heart. The technique can involve using radio waves (usually) to target the route the abnormal rhythms take or the site they are being generated. This can interrupt or isolate them so they can’t influence the heart any longer. This is a growing area of clinical practice, but is not perfect. It can be very effective in some patients.
So what next?
I have started running again. Thanks for support from various club members. You’ll probably see more of me in Groups 3 and 4 in the coming weeks. I was surprised how much three weeks off took out of my legs! I have stopped the beta blockers now (following advice) and will stay on the anticoagulants for a few more weeks. I need to be careful. I have taken a few tumbles in the past and that wouldn’t be great while on anti-coagulants. I am looking into buying a device called a Qardiocore, which offers the chance of continuous and real time monitoring of my ECG while exercising. Standard heart rate monitors don’t record a full ECG and would only help indirectly by showing sudden changes in heart rate. That can be useful and if you find that happening while using a Heart Rate Monitor, especially if you get any of the symptoms I’ve described, you should take it seriously. Feel your pulse and count how many beats per minute to check if the HRM is telling the truth. I was looking into the possibility of training for New York Marathon later in the year. One side effect of my diagnosis is a £250 rise in annual travel health insurance to visit the US. In part that has led me to the decision to stop running marathons. Overall I think my ambitions are going to be more about participating rather than competing. I am hoping that changing some of the things that had happened in my last training session – tiredness, inadequate lunch and late eating, alcohol – will allow me to do harder sessions without incident. Confidence like fitness is lost quickly and, I am finding, only comes back slowly!
Andy



9 Responses
Hi Andy,
Great reading. I myself suffer from AF and have done for about 5 years now. I didn’t know I had a problem, apart from feeling strange occassionaly during a run and suffering the odd dizzy spell. I couldn’t even feel my heart racing.
I had an over age 60 check at the doctors who sent me for an ECG where they found that my heart was running at over 160 beats to the minute. They tried cardioversion which did not work and as they can only do this again if it was a success first time around and, after numerous tests, they put me on 3 drugs, dabigatran, digoxin & dilzem which I still take. Apart from being enlarged, there is nothing else wrong with my heart and I was advised to continue running as long as was possible. I still have the odd dizzy spell due to my BP falling too low but as I now know what the cause is, it is less distressing now. The only thing I have to remember is that, when I run in the morning, to take my medication after the run otherwise my BP can be problematic.
The hardest part that I had to come to terms with was that I couldn’t run as fast as before as the drugs prevent my heart going too fast which was (and still is) frustrating. However, at 67 and also a cancer survivour, I now count myself lucky that I can still run.
Interesting to hear your experience Ron. I can understand how you might not have identified it yourself. That’s why I think that there is a huge gap in the market for a heart rate monitor that tracks ECG and is practical for runners.
Neither my GP nor my consultant could say for sure how long I had suffered with the condition. I still can’t feel the irregular heartbeat, even whilst running except occaisionally at night when resting in bed. It’s interesting about alcohol as I was never advised to stop drinking. Having said that, apart from the odd glass of wine or beer, I only really drink when on holiday. However, it does give me food for thought.
You are right in saying that it is also a matter of confidence. I still have times when I worry about trying to push myself too hard during a session. Also, I don’t think I’ve ran further than 10 miles since diagnosed. It’s not that I don’t want to, rather that tiredness kicks in and my body prevents me from doing so. It has taken me a long time to come to terms with the situation, that’s why I became involved with the coaching at the club. I take pleasure now in helping to bring other people on and seeing them progress through the groups.
My consultant, Mr Haq at the RVI, did some research whilst treating me and he found what you have detailed, that AF is very common in high performance athletes and he told me that my condition was probably caused by a combination of being on thyroid replacement drugs and having kept a very high level of fitness forover 30 years.
Did they discuss ablation with you?
Hi Andy,
Mr Haq decided that this wasn’t an option as my condition wasn’t life threatening so have been on meds ever since
Wow fascinating reading thanks for sharing your story I was born with a defect
Very interesting read and plenty to consider.
Thanks for sharing this, Andy.
Great article Andy.
I have had a few issues with Palpitations recently as well so found it really useful. Thankfully my ECG was fine and can train as normal. I am in my late 30’s so although it’s more likely with older runners, everyone should get themselves checked if it happens to them.
In my opinion, everyone should have their heart checked before starting physical exercise no matter their age